Diabetes and eyesight
Introduction
Diabetes is a disease resulting from the insufficiency or deficient metabolic effects of insulin. The first description of this disease ascends to Ebers’ papyrus in ancient Egypt, where it is defined as “disease of an excess of sweet urine associated with emaciation and death”. But it is a disease of modern societies, in which there is an adulteration of dietary habits and an excessive tendency for sedentary life.
Definition
The main symptoms of diabetes are: much thirst (polydipsia), frequent urination (polyuria) and loss of weight; there are often complaints of blurred vision. The diagnosis is confirmed through laboratorial tests, by a level of glycaemia above 200 mg/dl, subject to a second analysis. Depending on the age at onset and the clinical condition of the patient, there are two fundamental types of diabetes (type 1 – insulin-dependent, and type 2 – non insulin-dependent) with very different prognosis.
Ophthalmological consequences
The most serious ophthalmological consequence is diabetic retinopathy (DR), but all segments of the visual system may be affected. Starting from the ocular surface, the sensitivity of the cornea is frequently reduced, with propensity to keratitis, neurotrophic ulcers and persistent epithelial defects; corneal alterations are especially frequent after an ocular surgery, often with complications caused by the longer delay in cicatrizing. The most notorious alteration of the anterior segment, with the greatest social and economic impact, is cataract, 4 times more frequent in diabetics. The risk of cataract increases with disease continuity and with an inadequate metabolic control. Besides cataract, the crystalline lens may be affected by sudden variations of glycaemia levels, causing blurred vision due to refractive alterations, often fluctuant, resulting from sorbitol accumulation.
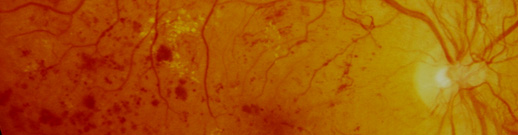
Why are diabetics at risk of blindness?
The main cause of blindness due to diabetes is DR. It begins with a unique biochemical alteration: the increase of blood serum glucose. Then, other biochemical alterations follow, that result in structural changes of the basement membrane of retinal capillaries, endothelial cells and pericytes. It ends with the rupture of the blood-retinal barrier, leading to macular oedema and alterations of blood circulation, with ischaemia, the consequence of which is the development of neovascularization. Macular oedema and retinal neovascularization are the specific causes of blindness due to diabetes.
Factors of risk of diabetic retinopathy
After 15 years with diabetes, DR is present in 97.5% of type 1 diabetics (the proliferative form in 67.5%) and in 77.8% of type 2 diabetics (the proliferative form in 15.5%).
The factors of risk are: the duration in time of diabetes, age, the level of glycated haemoglobin and high blood pressure. After 20 years with diabetes, macular oedema is present in 29% of type 1 diabetics and in 28% of type 2 diabetics. The factors of risk are: the duration in time of diabetes, the levels of glycated haemoglobin, proteinuria and high blood pressure.
Treatment
DR treatment is based on two main interventions: the treatment of the systemic disease and of the factors of risk, and the treatment of retinal complications.
As for the treatment of the disease, an adequate metabolic control is fundamental: intensive treatment reduces by 25% the appearing of lesions and by 75% their progression.
The treatment of other identified factors of risk, such as arterial hypertension and dyslipidaemia, is also very important.
As for the treatment of retinopathy proper, the most effective method is still laser photocoagulation, which destroys ischaemic retina and thus reduces the production of biochemical mediators, especially “vascular endothelial growth factor” (VEGF), capable of leading to the development of structural alterations and blindness. In case of macular oedema, laser treatment is localized and is intended to delay the loss of visual acuity: sight decrease falls from 24% to 12%. In cases of ischaemia and neovascularization of the retina, it is used panretinal photocoagulation (laser treatment of large areas between the vascular arcades and the equator). This procedure enables to reduce by more than 50% the risk of blindness in patients with proliferative DR and to induce a regression by 70 – 90% of preretinal or papillary neovascularization.
In the most severe cases of DR with fibrovascular proliferation and/or retinal detachment, the treatment is surgical and should always be performed in specialized centres with surgeons very differentiated in this type of surgery.
With the growing understanding of the physiopathological mechanisms of DR, particularly the fundamental role of VEGF, some very promising medicines are now used to inhibit vascular proliferation and alterations of vascular permeability. Anti-angiogenics, and particularly Aptamer-Pegaptanib and the monoclonal antibodies Bevacizumab (IgG) and Ranibizumab (antigen binding fragment – Fab), have been effective in the treatment of neovascularization that occurs in senile macular degeneration, and probably in the future they will be very useful in the treatment of vascular proliferation caused by diabetes.
Finally, all diabetics should be submitted to ophthalmological examinations periodically, according to clinical results. In type 1 diabetes, the onset of the disease is usually known with precision, and since DR appears in average 7 years later, the initial examination is not very urgent; nevertheless, after 20 years of evolution of the disease, 90 – 95% of the patients present DR and should be rigorously monitored. In type 2 diabetes, the onset of the disease is many times unknown, and so the patients should be immediately examined; in fact, the first examination may reveal lesions due to DR in 20% of the cases. Subsequently, the frequency of the examinations should be determined by the ophthalmologist, depending on the clinical condition of each patient. But there are periods of increased risk of development of DR, which require more care: in puberty and adolescence (DR development before this age is rare), during pregnancy, during a rapid equilibrium of glycaemia (the beginning of the treatment with insulin is many times related to the appearing of DR), after cataract surgery and during tensional or renal decompensation.