The tear is produced by the lacrimal glands: the normal daily production of this fluid being 10 millilitres. Most part of the tear flows, by gravity action, along the ocular surface, and is accumulated at the bottom of the lower conjunctival sac. From there, it is spread up by the blinking movements of the upper eyelid. This way, the outer surface of the eyeball is kept perfectly moistened by a lacrimal film, which in normal conditions has a homogeneous thickness.
The closing movements of the eyelids push the tear down, towards the inner corner of the eye. There, in a triangular space named lacrimal lake, the tear is accumulated. In the outer vertices of that space, two orifices named lacrimal puncta are the tips of the upper and lower lacrimal ducts. By pressure mechanism, the tear is drawn into the lacrimal sac through the upper and lower canaliculi (80% of the tear flows off through the lower canaliculus), and from there it is drained to the nasal fossa through the nasolacrimal duct.
Embryology
The precursory structures of the draining lacrimal system are differentiated in the embryo with 28 – 30 millimetres. Initially, these structures are solid cords. Subsequently, during their growth, they develop an inner space by a mechanism of cellular resorption, originating tubular elements. This ducting process begins in the lacrimal sac, around the 4th month, and afterwards it evolves to the development of the canaliculi and the upper part of the nasolacrimal duct. Finally, the nasolacrimal duct progresses downward to the membrane that separates it from the nasal fossa. The ducting process is completed around the 7th month of gestation and it coincides with the separation of the two eyelids.
In about 60% of the neonates, the membrane which separates the lacrimal tract from the nasal fossa persists after birth, preventing draining off. Nevertheless, most of the times, it perforates spontaneously during the 1st month of life.
Congenital obstruction of the nasolacrimal duct
It is by far the most frequent alteration of the lacrimal system in children, occurring in about 6% of them. In 1/3 of the cases the obstruction is bilateral.
It is, almost always, the result of the non-perforation of the membrane which separates the nasolacrimal duct from the lower meatus of the nasal fossa.
Signs and symptoms
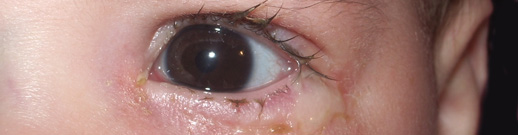
Characteristically, parents perceive the existence of mucous or mucous-purulent secretion on the conjunctiva or on the eyelashes of the baby, during the first days or weeks of its life. This is more evident in the morning, when the child awakes, or after sleeping periods.
Typically, the conjunctiva remains not inflamed, white, despite the existence of secretion, and this fact helps to exclude the presence of conjunctivitis.
The excess of tear fluid accumulated at the bottom of the conjunctival sac, although persistent, is usually unnoticed by the parents. But an attentive observation allows the examiner to perceive the moisture of the eye. With the help of light, it is possible to ascertain the existence of a tear lake or a tear meniscus on the joining of the posterior border of the lower eyelid with the eyeball. In spite of this moisture, the overflow of tear fluid onto the face is rare. Some adjuvant factors that increase tear secretion, such as cold or wind, can cause a superabundant lacrimation.
Also, the pressure exerted on the lacrimal sac may produce a reflux of mucous secretion onto the ocular surface, but this sign is not necessary to make the diagnosis.
Evolution
More than 90% of the cases of obstruction of the nasolacrimal duct are spontaneously solved before the age of 8 – 9 months. During this period, usually only medical treatment is applied. When the obstruction persists beyond this age, the possibility of probing the lacrimal tract should be considered.
Complications
The most frequent complication is dacryocystitis, an infection of the lacrimal sac requiring urgent treatment because it may quickly develop into preseptal cellulitis, orbital cellulitis or even sepsis.
Treatment
Treatment is decided depending on the child’s age and the severity of the symptoms. Usually, paediatricians or family physicians take upon themselves the responsibility of treating the baby until the age of 6 months, if there are no complications.
> Medical treatment
During this period, treatment should consist in massaging the lacrimal sac and applying an antibiotic collyrium. Topical antibiotics reduce the infectious component, many times present, but have no effect on the obstruction of the nasolacrimal duct! So, if there is no infection, their use is not necessary, though an application once a day is possible.
In case of purulent secretion, they should be applied several times a day.
How should the massage be performed?
First, the lacrimal sac should be cleaned, pressing it with a finger and sliding the finger upwards, in order to expel all the mucous and/or purulent secretions from the sac. Then the nasolacrimal system should be tightly massaged downwards. This technique forces the remaining fluid to exert pressure on the membrane that causes the obstruction. This procedure should be repeated 3 or 4 times, and it should be performed several times during the day.
> Surgical treatment
Probing of lacrimal tract.
The decision of probing the lacrimal tract should be taken depending on the severity of the situation, the child’s age and general health condition, and the anxiety of the parents.
When complications occur, such as dacryocystitis (an infection of the lacrimal sac), probing should be performed after the regression of inflammatory signs.
If the obstruction is not spontaneously solved but no complications arise, setting the right moment to probe the lacrimal tract causes many times controversy. Generally, it seems wise to perform it before or around 1 year of age. Despite the inexistence of unanimity of opinions, when performed later, probing success seems to decrease progressively with age.
Although it is possible to perform it under local anaesthesia and by immobilizing the baby, it is preferable to do it under general anaesthesia or sedation.
How is probing performed?
After dilating the lower and/or upper lacrimal punctum (orifice of the lacrimal duct), the ophthalmologist introduces a metallic probe through the respective canaliculus as far as the lacrimal sac. Then, rotating the probe to make way towards the nasolacrimal duct, he pushes it to the nasal fossa. Sometimes there are points of resistance to probing (generally at the end region, where the obstruction is more frequent), which easily yield to pressure. This operation should be performed initially with a very thin probe and subsequently with probes of greater calibre. To end the procedure, the lacrimal tract can be irrigated with a liquid dye (for example, Betadine®), the drainage of which is verified by pumping out the nasal fossa.
In the post-operative period, an antibiotic collyrium should be applied for one week. Some ophthalmologists prescribe a systemic antibiotic for several days, though not necessary, in order to prevent secondary infections.
The success rate of this probing varies usually between 80% and 90%. In case of recurrence of symptoms, a new probing can be performed, 3 to 6 months after the first one, or a bicanalicular intubation can be then carried out. It consists in introducing a silicone tube in both lacrimal ducts, joining at the nasal fossa where they are fixed.
There are also intubation systems for only one of the ducts (“Monoca”) and dilation systems for the nasolacrimal duct in its point of stenosis (“LacriCATH”). In case of persistence or recurrence and of repeated dacryocystitis, the treatment consists in a dacryocystorhinostomy (DCR).
Absence of lacrimal puncta.
It is a rare situation in which the lacrimal ducts are not patent, not externalized in the border of the eyelid. Sometimes, they are obstructed only by a very thin membranous structure which is easily ruptured; other times, a more complex intervention is required to open them.
Congenital fistula
It consists of a fistulous passage between the lacrimal sac and the skin, or between the common canaliculus (resultant of the joining of the upper and lower canaliculus before draining into the lacrimal sac) and the skin. In these cases, a small orifice is visible in the skin, from which tear fluid, mucus or pus spontaneously flows. It may need surgical correction.